From GI Roundtable 29: Is Your Health the Nation’s Business? (1946)
Five key pillars are necessary to support national health according to these reports. They are: (1) distribution of the costs of health services, (2) establishment of hospital and public health facilities, (3) organization of medical service: to promote a high quality of care, (4) administration satisfactory to patients and the professions, and (5) promotion of continued scientific research and education.
Distribution of costs
Starting out with the twin assumptions that the present individual pay-as-you-go method of meeting medical costs has proved itself unsuited to the needs of the population and that voluntary insurance is too limited in scope, advocates of national health program recognize two alternative ways of meeting medical costs. Both methods of payment are based on the fact that while individuals can never predict when they will be sick or how expensive their illnesses will be, the expected incidence of illness for large groups of people and its costs can be fairly well determined. By chipping in regularly to a common pool amounts which are fair in proportion to his income, each member of the large group can be sure that there will be funds to pay for his own health needs, whether large or small, whether they occur next year or tomorrow.
The first alternative is a system of national health insurance, combined with support from general tax funds. This method is advocated in both reports. National health insurance is no new thing, in fact it is in operation in thirty-one nations. In some it is over fifty years old. It works like this: Employed people turn in a certain part of their wages each month, through payroll taxes, to a government-administered health insurance fund. Employers match the amounts each worker puts in, as under Social Security in the United States. When sickness strikes the wage earner or his family, doctor and hospital bills are paid out of the insurance fund.
Insurance of this type was designed originally for the wage earner, whose premiums can be easily collected through pay-roll deductions and for whom employers can also make their contributions easily. Such health insurance in other countries has seldom been available to farmers, people who run their own small businesses, domestic servants, and other similar occupation groups. Health insurance on this plan does not touch the sickness costs of nonworking people-the unemployed, the aged, the chronically ill. For this reason both the ‘‘A.P.H.A. and the Health Program Conference reports recommend that, if national health insurance is adopted, it be supplemented by general tax funds to include all groups of the population.
The second alternative method of financing, suggested by s the A.P.H.A., is that the insurance features be forgotten and public health services be paid for simply and solely out of ‘taxes-just like public schools. This, it is argued, would involve far less red tape. All groups of the population would pay for their health services by the same kind of taxes. The amount would vary according to the particular circumstances of the individual. Great Britain, which has had national health insurance since 1911, is planning a system in which two-thirds of the costs will be financed through general taxation along these lines.
\Whichever may be the better way of enabling people to pay for medical care-whether by health insurance combined with taxation or by taxation alone-the reports of the A.P.H.A. and the Health Program Conference agree that as long as payment is made in the manner of today, the “right to achieve and enjoy good health” will not be truly available to all, and that some such nation-wide solution must be found for the problem.
But a method of paying for medical care is only part of the story. With a thousand dollars in his pocket, a man on a desert island with no doctor or hospital could still not get his broken arm set. Both the A.P.H.A. and Health Program Conference plans emphasize the need, for construction of facilities in areas which lack them and improvement and enlargement of facilities where they are inadequate.
Facilities and personnel
The keystone here, according to both reports, is the hospital. A hundred years ago the hospital was mainly a place for the sick poor to go, often only to die. Today, the hospital is a place to which any sick person goes to get modern treatment, and it is a place where he expects to get well.
The hospital is indispensable in practice to the provision of good medical care-yet 40 percent of the counties of the United States have no recognized hospital facilities. This situation would be bad enough in itself; yet it is also reflected in the number and kind of physicians such counties can attract. Younger physicians whose education and training is centered in well-equipped and well-organized hospitals cannot practice the kind of medicine they have so painstakingly learned in school unless there is a hospital to work in.
The result is that counties with no general hospitals have only half as many doctors per thousand inhabitants as counties of the same income level which are generously supplied with hospitals. Since counties lack hospitals directly in proportion to their inability to support them, those who favor a national health program think that federal funds should be used to construct, enlarge, and modernize hospitals in the poorer counties.
The A.P.H.A. report, in addition to urging hospital construction, stresses the need for public health departments to serve all areas of the country. At present, 1,223 of the nation’s 3,000 counties lack any organized health department.
The need has long been generally recognized for health departments to insure safe water and milk supplies, sewage disposal, and control of communicable diseases, and for health centers where special clinics can be conducted, such as those for maternal and infant care or diagnosis and treatment of venereal disease. The A.P.H.A. report again emphasizes this need and concludes that it should be woven into a national health program.
Both reports assume that modern hospital and public health facilities, combined with improved methods of paying for needed medical services, would, to a certain extent, automatically attract doctors, dentists, and nurses to areas which are now greatly undersupplied.
Organization of services
With a fairer way of paying the health bill and with hospitals and medical personnel distributed according to where they are needed, many of the objectives of a national health program would be realized. What about the quality of this care? Obviously, quality under any system of financing is, in the last analysis, what the individual doctor, nurse, dentist, or laboratory technician makes it. Nevertheless, certain methods of organizing professional services tend ‘more than others to encourage advances in quality.
The report of the A.P.H.A. and, more particularly, that of the Health Program Conference, stress encouragement of better professional organization as another essential of a national health program. The focus here, again, is the hospital but a hospital that functions in a new and different way. It is to become not only a place where illness is treated, but also a center for preventing disease and for improving the whole practice of medicine in the surrounding area. It is suggested that such a truly modern hospital could, in addition to its usual facilities, house public health clinics, the offices of physicians and dentists, and. equipment for the common use of all. In such a group-practice unit, doctors would be encouraged to work more as a team, pooling their knowledge and skills.
Group practice
The general physician, it is assumed, would be the patient’s plain source of medical care. But at his elbow would be the hospital and the specialists whose services are necessary if he is to practice modern medicine. Freed through health insurance from the responsibilities of fee setting and bill collecting,
The family doctor might, for example, find more time to act as a guide and counselor in the emotional problems of his patients as well as providing them with other types of medical care. His role in the prevention of mental illnesses, one of our biggest unmet health needs, might be strengthened through the advice and teaching of his colleagues in psychiatry.
Working in groups, doctors are to some extent supervised by, each other in the kind of services they render. For example, a young surgeon in a group is usually assisted by a more experienced colleague when undertaking an especially ticklish operation. The story leading up to the death of any patient is reviewed at staff meetings. These supervisory practices are not a new idea; they have been used for years in good hospitals to safeguard the quality of medical service, especially for ward cases.
Such supervision does not require an outside government inspector. Under any health program it could be carried out, as at present, by groups of physicians themselves. Indeed, as mentioned before, group medical practice is no new idea, but a familiar phenomenon in the private group clinics scattered throughout the United States, particularly the middle western and western states. What is new° in the Health Program Conference report is the idea of encouraging this type of organization throughout the nation, and combining it with a more favored place for the family doctor than exists now either in individual or in certain types of group practice.
A network of hospitals
Towns and cities of different types, sizes, and locations naturally require different sized hospitals and differently equipped hospitals. The country hospital, for example, could never make enough use of radium to justify the expense of owning it. A thinly populated area may need a highly trained brain surgeon only once or twice a year. Nevertheless, when these and other unusual services are needed, they must be accessible. What is the answer?
Both reports endorse a plan of organization somewhat similar to that of Army hospitals. They would encourage future construction of hospitals according to an integrated scheme of health centers (corresponding to the Army field station)-rural hospitals, district hospitals, and base hospitals.
To illustrate: A state might have one or more base hospitals, preferably connected with medical schools, where all types of medical-service would be available and where the more unusual types of treatment would be carried out. Here, where they could answer any need in the state, would be the brain surgeons and the radium. Base hospitals would also be centers of teaching and medical research.
The many district hospitals, located in large towns or cities, would be large, and equipped to handle the more usual medical and surgical cases. Smaller rural hospitals would be far more numerous than at present and would be designed to take care of ordinary diagnosis and treatment, minor surgery, obstetrics, and so forth. They would refer complicated conditions to the district or base hospitals. Health centers, spotted about hospitals of all types, would house the offices of public health nurses, laboratories, public health clinics, doctors’ offices,-and some emergency beds.
Patients would, as a rule, go to the hospital nearest home, but for particularly difficult types of diagnosis or treatment might go to a base hospital, much in the same way that those who can manage it now go to a well-known clinic or medical center.
This scheme of integrated hospitals would make constant exchange of information, training, and personnel among them possible. On this foundation, a consultation service could be built so that at regular intervals specialists from the larger hospitals would visit rural hospitals and health centers. At the same time, rural physicians might go up to the base hospital for special postgraduate training, returning to their practice stimulated and better prepared.
Proponents of a nation-wide health program see in hospital organization along these lines a tremendous inducement to physicians to organize themselves into strong professional groups. Whether or not doctors would wish to take advantage of these opportunities would of course remain to be seen. There are indications that younger members of the profession, in particular, would welcome the chance.
Administration
How could such a program be carried out so that both the patients who receive the services and the doctors, dentists, nurses, hospital people, and others who render the services
would-be satisfied? Here, the guiding principle, both reports agree, is that while the health program should be national in scope and while certain national standards are necessary to insure that public funds are used to best advantage, nevertheless the responsibility for the detailed planning and working of the program must rest with local areas.
For example, the federal government might refuse to allot national health funds to hospitals without laboratories. Few would question that such minimum standards should be set. On the other hand, the government would not be similarly justified in trying to tell doctors when to use a particular kind of laboratory test. Such judgments must of course be made by the doctor himself, subject to the staff regulations of his fellow physicians in the particular hospital.
Except for professional questions, the lay public, which receives it, should have a strong say on how the service is conducted, both in their own communities and at the state and national levels:
Certain freedoms are considered basic
- Patients should be free either to make use of services provided under the national program or to continue to secure medical services in the traditional manner, as they prefer.
- Patients should be entitled to choose among individual physicians, organized groups of physicians, hospitals, and so forth. Likewise, they should be free to change their sources of service without difficulty.
- Physicians should be free, as they now are, to accept or reject patients; to participate or not to participate in a national program; to furnish services as individuals or to associate with other physicians in groups.
- Voluntary agencies (such as hospitals) should be encouraged to participate in the national program, maintaining their status as independent agencies and retaining full responsibility for their own administration, or not to participate in the national program if that is their preference.
Incomes of physicians
Neither the A.P.H.A. nor the Health Program Conference report offers a pat solution to the thorny question of how doctors should be paid. They agree that medical services should be provided as economically as is consistent with high quality. At the same time they feel that remuneration to doctors should be sufficient to attract and hold good men and should be scaled so that there are financial rewards for professional excellence.
There are three principal ways doctors could receive payment under a national health program. The health fund could pay doctors in individual practice: (1) a fee for each service rendered to patients, in the same way that most doctors now collect fees from their private patients, or (2) a set amount per year, called a “capitation fee” for each person choosing the doctor’s services. Doctors working together in group practice could be paid by salaries from their groups. In such cases the health fund could pay (3) a lump sum to the organized group, determined by the extent of medical service the group provided or the number of patients using it.
Although fee-for-service is most used in private practice today, there are also many physicians in the United States who are paid by the other methods and apparently find them satisfactory. When faced with the prospect of payment by the government, however, doctors are naturally concerned lest they be underpaid. Medical education is expensive, and it takes a number of years after graduation before doctors begin to earn a living by their practice. It is natural for doctors to wonder whether a government system would offer a reasonable income. The example of poorly paid schoolteachers, government clerks, public health nurses, and “city physicians” does not reassure them. Many people feel that the question of payment to physicians lies at the heart of doctors’ opposition to a national health program.
Both the A. P. H. A. and the Health Program Conference reports agree that there is room for experimentation with methods of paying physicians, but argue that a physician’s yearly income must be adequate, as, measured by the incomes usual among other physicians of the same age and training and in the same type of community, and by the incomes of other professional groups.
Research and education
Under any type of health program, the quality and the continued improvement of medical services lean heavily on re-search and medical education. The half billion dollars invested in these fields by private philanthropy over the last fifty years are held to be largely responsible for the high place of American medical science today. Advocates of a national health program say that government funds must be forthcoming where private funds leave off if knowledge is to march steadily forward. In fact, during the war, the federal government sponsored and in many cases subsidized both medical and nursing education and a variety of scientific research. The results-for example, discoveries as to the processing and uses of stored blood-are familiar enough to those in the armed forces.
In addition to funds for research, the Health Program Conference report emphasizes the need for more opportunities for postgraduate training for physicians. Medical science advances so rapidly that the physician who graduates from medical school this year will find it necessary next year to bring himself up to date. Too often the busy practitioner has do time to keep up with advances through study and reading; rarely is he in a position where he can afford to take a month off for postgraduate study. This is particularly true of the country doctor. Opportunities for doctors to get postgraduate medical education could be greatly furthered by the use of public funds, advocates claim, although even more important day-by-day results would be obtained through improved organization of medical services.
The OSRD report
The use of federal funds to support a program of scientific research was recommended to President Truman in July 1945 in a report of Dr. Vannevar Bush, director of the Office of Scientific Research and Development-the government agency responsible for the use of federal funds for such research during the war.
In this report the war against disease is given first consideration. Dr. Bush strongly advocates government support of medical research as basic to any national program of expanded medical training and research and to the promotion of public health.
The report, which recommends the establishment of a national scientific research foundation responsible to the presi-dent and Congress, was received with widespread public interest.
Next section: Has a National Health Program Been Put before Congress?
Related Resources
September 7, 2024
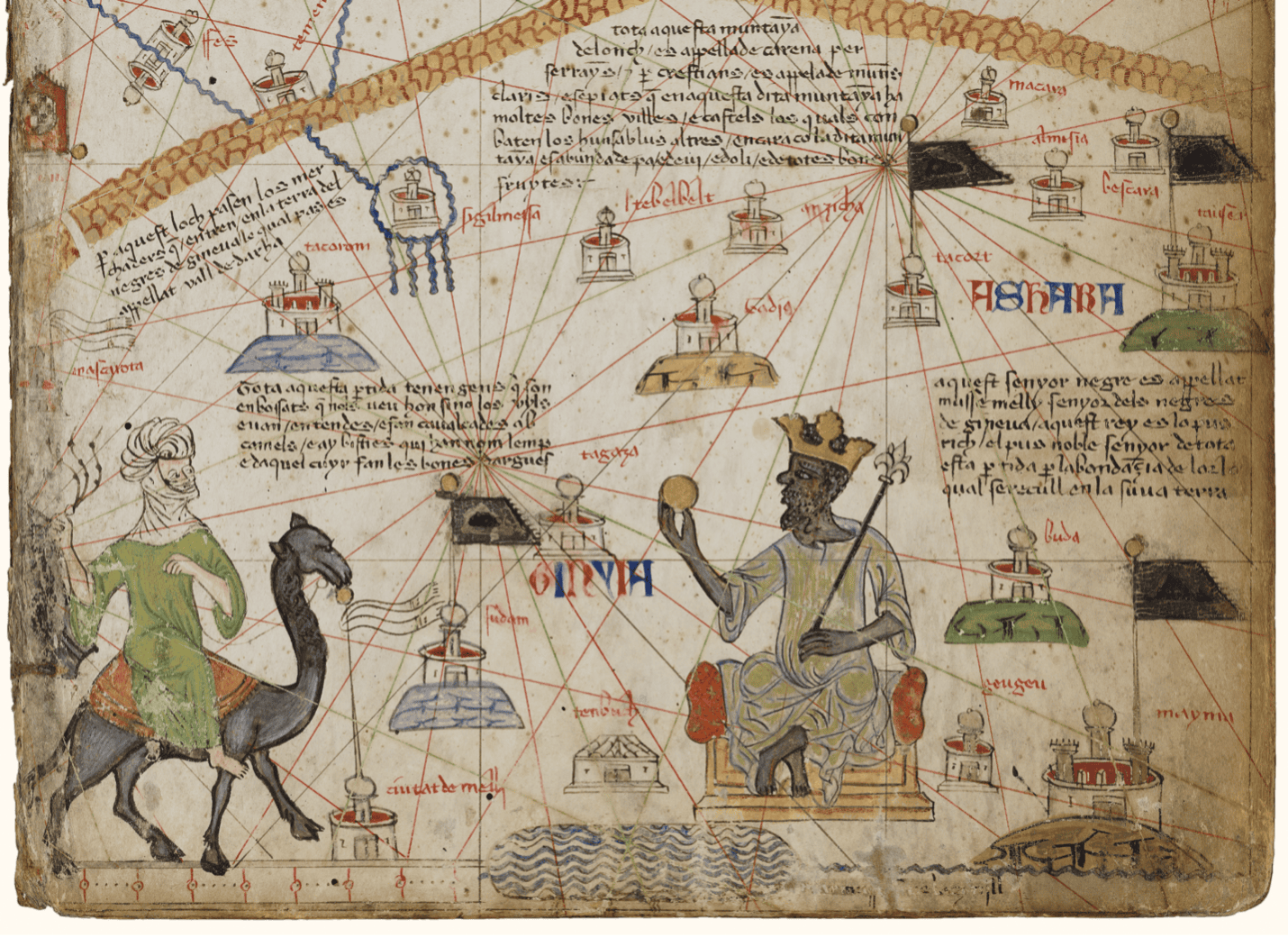
Travel and Trade in Later Medieval Africa

September 6, 2024
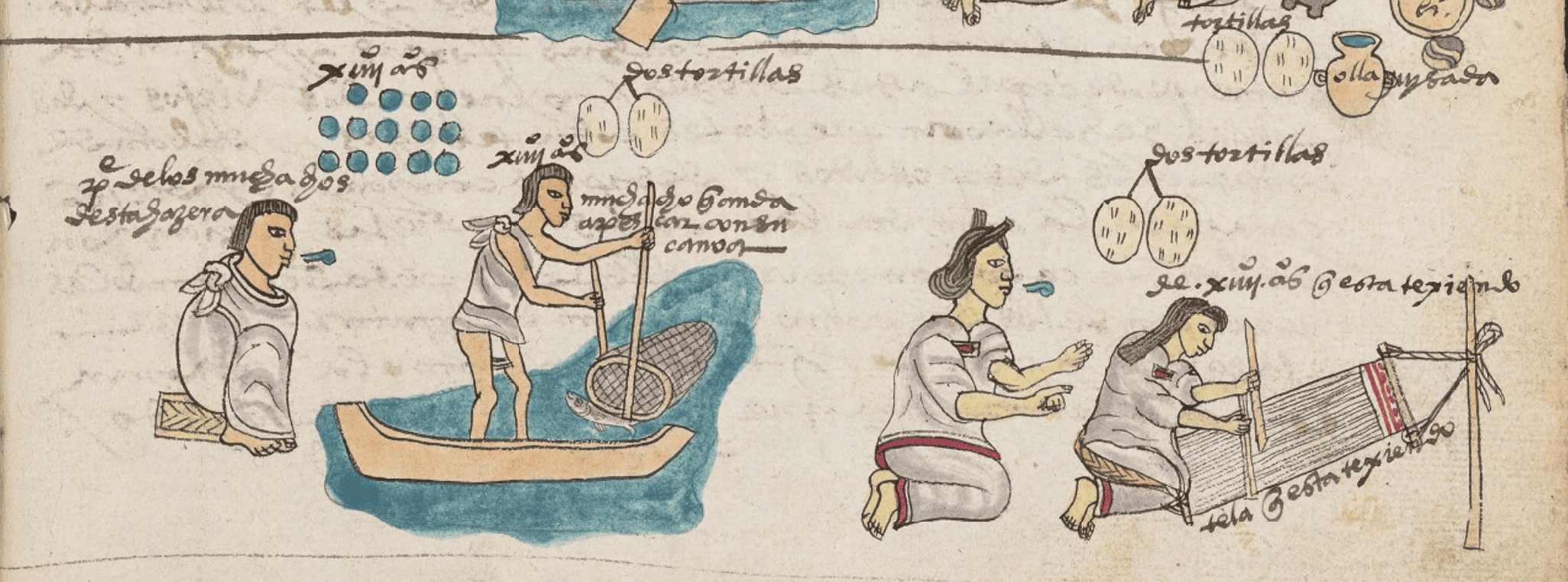
Sacred Cloth: Silk in Medieval Western Europe
September 5, 2024